特应性皮炎严重的后果
特应性皮炎对儿童和青少年健康的影响


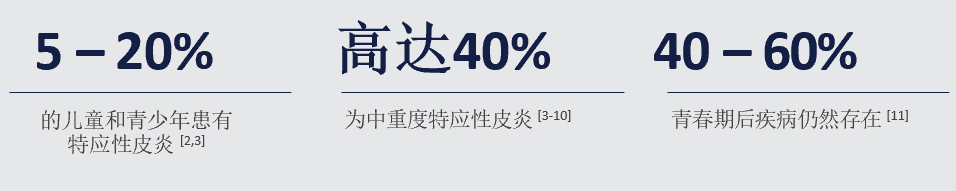
特应性皮炎是湿疹的一种形式,是影响儿童和青少年最常见的皮肤病之一。[1]
特应性皮炎是一种慢性炎症性皮肤疾病,由过度活跃的免疫反应引起,称之为2型炎症。[12,13]

儿童和青少年患者可能会出现症状复发,并经历频繁的急性发作
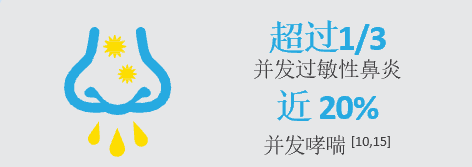
儿童和青少年患者经常伴有其他由2型炎症引起的特应性疾病,从而增加了总体疾病负担。
特应性皮炎对儿童和青少年以及家庭的影响
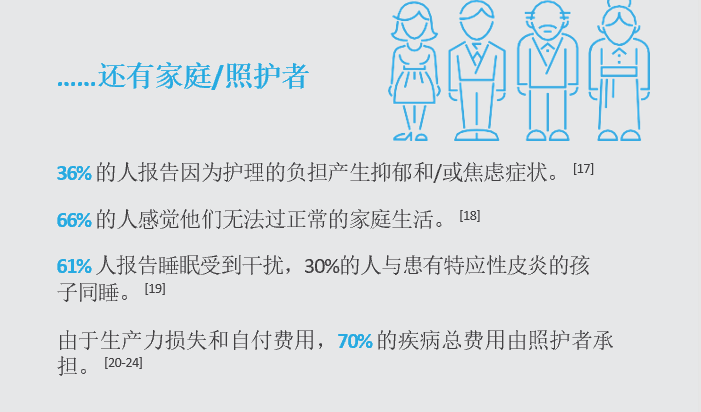
特应性皮炎患者带病生活的影响远远超出了皮肤,它会影响整个家庭。
特应性皮炎不仅是一种皮肤疾病,它的身体负担会严重影响儿童和青少年,以及整个家庭的生活质量。
01、儿童和青少年

02、家庭和照护者
让我们共同努力,敦促采取政策行动,通过疾病教育、更好的护理和及时获得正确的治疗,解决中重度特应性皮炎患者未得到满足的需求。通过这些行动,我们可以减少特应性皮炎对儿童、青少年及其家庭的身体、情绪和社会影响。
参考文献
1. R. J. Hay, M. Augustin and C. E. Griffiths, “The global challenge for skin health,” Br J Dermatol, vol. 172, no. 6, pp. 1469-1472., 2015.
2. T. E. Shaw, G. P. Currie and C. W. Koudelka, “Eczema prevalence in the United States: data from the 2003 National Survey of Children’s Health,” J Invest Dermatol, vol. 131, no. 1, pp. 67-73, 2011.
3. H. Williams, C. Robertson and A. Stewart, “Worldwide variations in the prevalence of symptoms of atopic eczema in the International Study of Asthma and Allergies in Childhood,” J Allergy Clin Immunol, vol. 103, no. 1 Pt1, pp. 125-138, 1999.
4. N. Ballardini, I. Kull and C. Soderhall, “Eczema severity in preadolescent children and its relation to sex, filaggrin mutations, asthma, rhinitis, aggravating factors and topical treatment: a report from the BAMSE birth cohort,” Br J Dermatol, vol. 168, no. 3, pp. 588- 549, 2013.
5. S. J. Brown, C. L. Relton and H. Liao, “Filaggrin null mutations and childhood atopic eczema: a population-based case-control study,” J Allergy Clin Immunol., vol. 121, no. 4, pp. 940-946 e 943, 2008.
6. S. Dhami and A. Sheikh, “Estimating the prevalence of aero-allergy and/or food allergy in infants, children and young people with moderate-to-severe atopic eczema/dermatitis inprimary care: multi-centre, cross-sectional study,” J R Soc Med, vol. 108, no. 6, pp. 229- 236, 2015.
7. A. Lebon, J. A. Labout and H. A. Verbrugh, “Role of Staphylococcus aureus nasal colonization in atopic dermatitis in infants: the Generation R Study,” Arch Pediatr Adolesc Med, vol. 163, no. 8, pp. 745-749, 2009.
8. A. B. Olesen, K. Bang and S. Juul, “Stable incidence of atopic dermatitis among children in Denmark during the 1990s,” Acta Derm Venereol, vol. 85, no. 3, pp. 244-247, 2005.
9. H. Saeki, H. Iizuka, Y. Mori and et al, “ Prevalence of atopic dermatitis in Japanese elementary schoolchildren,” Br J Dermatol, vol. 152, no. 1, pp. 110-114, 2005.
10. J. I. Silverberg and E. L. Simpson, “Association between severe eczema in children and multiple comorbid conditions and increased healthcare utilization,” Pediatr Allergy Immunol, vol. 24, no. 5, pp. 476-486, 2013.
11. B. Wuthrich, “Clinical aspects, epidemiology, and prognosis of atopic dermatitis,” Ann Allergy Asthma Immunol, vol. 83, no. 5, pp. 464-470, 1999.
12. B. E. Kim, D. Y. Leung and M. Boguniewicz, “Loricrin and involucrin expression is down- regulated by Th2 cytokines through STAT-6,” Clin Immunol., vol. 126, no. 3, pp. 332-337, 2008.
13. D. Y. Leung and E. Guttman-Yassky, “Deciphering the complexities of atopic dermatitis:shifting paradigms in treatment approaches,” J Allergy Clin Immunol, vol. 134, no. 4, pp. 769-779, 2014.
14. T. Zuberbier, S. J. Orlow and A. Paller, “Patient perspectives on the management of atopic dermatitis,” J Allergy Clin Immunol., vol. 118, no. 1, pp. 226-232, 2006.
15. N. A. Gandhi, B. L. Bennett and N. Graham, “Targeting key proximal drivers of type 2 inflammation in disease,” Nature Reviews, Drug Discovery, vol. 15, no. 1, pp. 35-49, 2016.
16. Eczema Society of Canada, “Atopic dermatitis quality of life report. Moderate-to-severe disease. 2016/2017 survey results,” [Online]. Available: https://eczemahelp.ca/wpcontent/ uploads/2017/09/ESC_QUALITY_OF_LIFE_REPORT_2017.pdf.. [Accessed 3 May 2019].
17. A. Manzoni, M. B. Weber and A. R. Nagatomi, “Assessing depression and anxiety in the caregivers of pediatric patients with chronic skin disorders,” An Bras Dermatol, vol. 88, no. 6, pp. 894-899, 2013.
18. U. Gieler, S. Schoof and T. Gieler, “Atopic Eczema and Stress among Single Parents and Families: An Empirical Study of 96 Mothers,” Acta Derm Venereol, vol. 97, no. 1, pp. 42-46, 2017.
[19. S. L. Chamlin, C. L. Mattson and I. J. Frieden, “The price of pruritus: sleep disturbance and cosleeping in atopic dermatitis,” Arch Pediatr Adolesc Med., vol. 159, no. 8, pp. 745-750, 2005.
20. M. G. Filanovsky, S. Pootongkam, J. E. Tamburro and et al, “The Financial and Emotional Impact of Atopic Dermatitis on Children and Their Families,” J Pediatr, vol. 169, pp. 284-290, 2016.
21. D. Fivenson, R. J. Arnold and D. J. Kaniecki, “The effect of atopic dermatitis on total burden of illness and quality of life on adults and children in a large managed care organization,” J Manag Care Pharm., vol. 8, no. 5, pp. 333-342, 2002.
22. J. C. Su, A. S. Kemp and G. A. varrigos, “Atopic eczema: its impact on the family and financial cost,” Arch Dis Child, vol. 76, no. 2, pp. 159-162, 1997.
23. D. R. Bickers, H. W. Lim and D. Margolis, “The burden of skin diseases: 2004 a joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology,” J Am Acad Dermatol, vol. 55, no. 3, pp. 490-500, 2006.
24. R. M. Emerson, H. C. Williams and B. R. Allen, “What is the cost of atopic dermatitis in preschool children?,” Br J Dermatol, vol. 144, no. 3, pp. 514-522, 2001.
内容来源:中国AD之家
